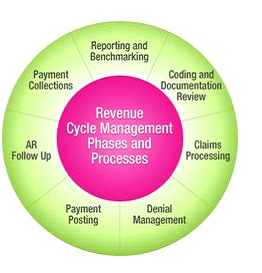
Squadm is an advanced medical billing management solutions for the US healthcare industry with proven track record of 100% HIPAA compliant. Our End to End services focus on the entire revenue cycle including validating demographics and billing, to patient calling and reporting. Our Revenue Cycle Management (RCM) solution can help you to increase revenue, reduce costs and strengthen customer relationships. We need the Software platform and clearing house, we do the rest and make patient to cash cycle easy to our clients. Squadm provides the highest quality service while ensuring HIPAA compliance and process redundancy.
The Process of Registering Patient in to system, Enter patients personal Information from demographic sheet to EMR. Process charges for multiple specialties and be able to work according to regulations related to Medicare, Medicaid, Managed Care, Third Party Liability, Workers Compensation, Preferred Provider Organizations and Indemnity Insurers
Insurance eligibility verification is the most important and the first step in the medical billing process, lack of or improper insurance eligibility verification directly impacts the reimbursements. We Verify insurance eligibility and benefits for patients for free to minimizing the risk of claim denials.
Translating medical reports into a code using CPT, ICD-10-CM, and HCPCS Level II classification systems. Identifying and assigning specific codes for billable procedures. We providing a experience to our clients in an increase in returns and a reduction in the number of denials as we comply with the ICD-9-CM Official Guidelines for Coding and Reporting, AMA Guidelines from CPT-4 Code Manual CMS (HCFA) Guidelines [CCI (Correct Coding Initiatives)] and [LMRP(Local Medical Review Policies)].
Generating claim for a particular patient for the services provided and claims are submitted and filed with the respective insurance company. Analysing Clearing house rejections and errors sent back to the respective department and will be completed on the same day.
Applying payment in to the billing software against appropriate patient account. Cash posting includes comprehensive financial services offering superior payment convenience and flexibility. This includes the collection of co-payments, co-insurance, and deductibles while enabling the scheduling of automatic payments from a patients credit card.
Our Process tracks each and every claim and Quickly and easily determines the cause of denial, mitigate the risk of future denials, and get paid faster. Analyse the account receivable and identifies the patient account that require follow up. Appeal and claim Resubmission for the denial required Appeal and Resubmission will be reviewed on a daily basis and take necessary action within the insurance time Limit.
We Ensure Patient Statement Follow-up on a required time for the claims responsible for self-pay.
These include patient and provider wise details on the claim amount, receipts, total collections and outstanding amounts. Create reports for revenue, billing, insurance, claims, visit notes, outstanding statements